We have returned from our hiatus as of mid-august as expected!! check back frequently for updates!!
If you are using a mobile browser, please ensure you change your settings to display the desktop site for the time being!!
Long-Term Suboxone Treatment: Why Staying the Course Saves Lives
A dangerous misconception in recovery is that abstinence must be the end goal. Too often, people pressure others off Suboxone, calling it a “substitute” or “not real recovery”—even as many of those same voices struggle with relapse themselves. Some favor injections as “cleaner,” but they don’t work for everyone, and Suboxone is no worse. This stigma often reflects addictive thinking—black-and-white, fiending, and unresolved. With healing, that mindset fades. The evidence remains: Suboxone is safe, effective, and life-saving.
9/12/20254 min read
One of the most damaging ideas in addiction recovery is that abstinence should always be the end goal, with medication-assisted treatment viewed as temporary at best and shameful at worst. This belief often leads people in positions of influence to pressure others to come off Suboxone, insisting it is “just another drug” or “not real sobriety.” Many of these same voices, however, are chronic relapsers themselves. They often claim that MAT should only be a short bridge at the beginning of a persons recovery, and that it blocks "connection to God/a higher power". Their struggles do not make them unworthy of being heard, but it is dangerous when their perspective becomes the guiding message for others in recovery (especially those just beginning their journey in recovery).
The evidence is clear: people who remain on Suboxone do far better than those who taper off. In one landmark New England Journal of Medicine study, patients maintained on buprenorphine had longer periods of abstinence, higher retention in treatment, and fewer relapses compared with those who discontinued. The multi-site POATS trial confirmed that relapse was the overwhelming outcome for those who tapered, even with counseling support, while those who stayed on medication maintained stability. Another analysis published in The BMJ showed that patients on MAT cut their risk of all-cause mortality by more than 50%. These findings are not ambiguous; stopping Suboxone is not a sign of progress but a risk factor for relapse and overdose.
The danger of discontinuation goes beyond relapse alone. Studies show that the two weeks following cessation are especially deadly. During this period, tolerance drops quickly, but cravings remain, leaving patients at high risk of fatal overdose if they return to use. Research has also shown increased rates of suicide after stopping treatment. These are not personal failings, they are predictable medical outcomes of removing a protective medication.
Yet stigma persists, and much of it is aimed directly at Suboxone. Some in recovery circles view monthly injections like Sublocade or Vivitrol as “cleaner” or “less evil” than Suboxone films or tablets. But injections don’t work for everyone. As a matter of fact they made my life an utter hell on Earth compared to Suboxone which allowed me to feel human again. They can bring side effects, create cost barriers, and don’t always provide the consistent stabilization people need. To elevate injections while disparaging Suboxone isn’t medical reasoning; it’s a form of black-and-white thinking that reflects unresolved addictive mindsets. Addiction thrives on extremes: clean or dirty, good or bad, sober or not. When someone insists Suboxone is worse, it’s often because they are still fiending, moralizing, or projecting shame instead of facing their own unresolved trauma and pain. This doesn’t make them failures, but it does mean their healing is incomplete. The hopeful truth is that over time, with therapy, self-work, and growth, this distortion fades. People stop seeing medication as a crutch and begin recognizing it as what it is: a stabilizer that makes long-term recovery possible.
The reality is that Suboxone is not replacing one drug with another; it is a partial agonist designed to block euphoria and cravings while restoring balance to the brain. Some who are on Suboxone or other forms of buprenorphine may occasionally experience some side effects similar to the effects of their drug of choice, but these effects are much more mild and far less reinforcing and dangerous than those of their drug of choice. Long-term Suboxone use is safe for both brain and body. Far from causing harm, buprenorphine helps normalize disrupted pathways, reduces stress reactivity, and balances neurotransmitters that are often permanently altered by opioid use disorder. Patients consistently report improved mental health, lower anxiety, and more emotional stability while on maintenance. The idea that it damages the brain is not supported by evidence; in fact, studies show it helps the brain heal.
Professional organizations echo this consensus. The American Society of Addiction Medicine makes clear that there is no recommended time limit for buprenorphine treatment, and SAMHSA’s TIP 63 guidance emphasizes that discontinuation should only ever happen slowly and cautiously (if at all). What’s more, real-world outcomes consistently prove that patients who remain on MAT are safer and healthier: longer periods of abstinence, far lower relapse rates, dramatically reduced overdose risk, and more stable mental health as well as improved overall functionality in life.
Opioid use disorder is considered a chronic disease (whether one chooses to look at it as such or not, the underlying mechanisms are the same), and it should be treated as one. Just as no doctor would demand that a diabetic stop insulin, it is irresponsible and dangerous to push people off Suboxone in the name of “pure abstinence.” For some, injections may be the right fit. For others, daily Suboxone is what keeps them alive, stable, and rebuilding their lives. Neither path is inherently better, but both are valid. What matters is not the form of MAT but whether it works for the individual. The real danger is not in choosing Suboxone, but rather in the stigma that tries to take it away (no matter how subtle those that present such are about it).
The bottom line is this: Suboxone is not a detour from recovery. It is recovery. It saves lives, protects the brain, improves mental health, and reduces overdose risk. The stigma against it often comes from unresolved addictive mindsets, but those distortions fade with time and growth. What remains constant is the evidence: people who stay on Suboxone are safer, healthier, and far more likely to survive. The goal of recovery is not to satisfy ideology or purity tests, it is to stay alive. Suboxone makes that possible.
Outside Resources for Verification of Claims and Additional Insights
Primary Care–Based Buprenorphine Taper vs. Maintenance Therapy for Prescription Opioid Dependence
Adjunctive Counseling During Brief and Extended Buprenorphine–Naloxone Treatment for Prescription Opioid Dependence
Mortality Risk During and After Opioid Substitution Treatment: Systematic Review and Meta-analysis
Suicide Following Buprenorphine Treatment Discontinuation
Buprenorphine Treatment Retention and Mortality: A Multisite Cohort Study
ASAM National Practice Guideline for the Treatment of Opioid Use Disorder
TIP 63: Medications for Opioid Use Disorder
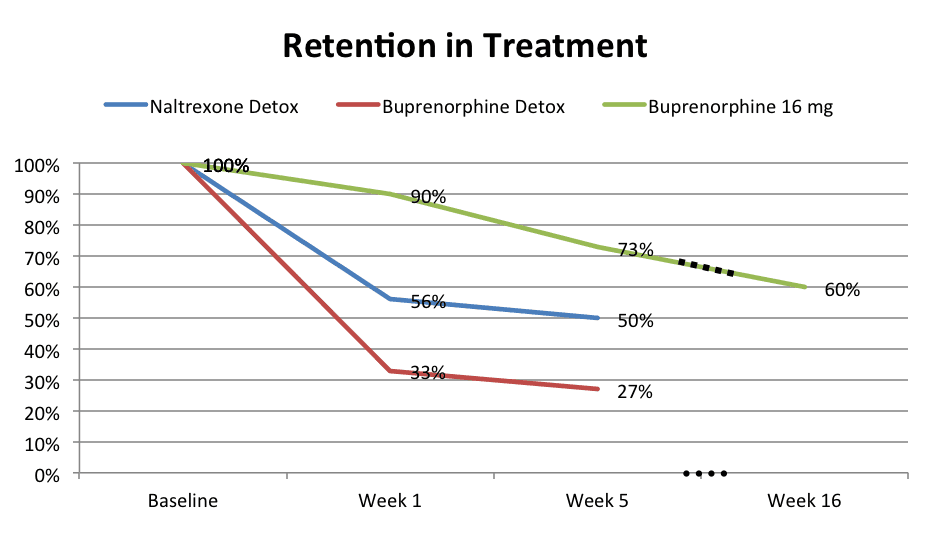
Chart adapted from: Sullivan, Maria, et al., American Journal of Psychiatry (2017)
As seen in the above, those who detoxed from opioids in this study using buprenorphine had the worst outcomes, second to those who detoxed using naltrexone. But, as is quite clear, those who continued on buprenorphine had remarkably high success rates in comparison to either.
