We have returned from our hiatus as of mid-august as expected!! check back frequently for updates!!
If you are using a mobile browser, please ensure you change your settings to display the desktop site for the time being!!
Access Denied: How Kratom Bans and Reduced Access to Suboxone May Fuel a New Epidemic
As kratom bans and restricted access to Suboxone limit safer alternatives, individuals are increasingly turning to a drug market contaminated with fentanyl, xylazine, and medetomidine. The rise of nitazenes—ultra-potent opioids resistant to naloxone—further escalates overdose risks. Without expanded treatment and harm reduction measures, the current drug crisis threatens to intensify.
9/4/20254 min read


The drug supply in the United States has never been more unstable, unpredictable, or deadly than it is today. The latest data from the National Drug Early Warning System’s Harm Reduction Organization (HRO) Network Report, Spring 2025 paints a troubling picture of what people who use drugs—and those tasked with treating the consequences of use—are facing in real time.
A Market Defined by Adulteration
Across the country, adulteration is the rule rather than the exception. In Florida, 89% of drug-checking samples tested this year contained harmful contaminants, with fentanyl and xylazine continuing to dominate the supply. New compounds like medetomidine are also appearing in multiple states, often layered into fentanyl, complicating reversals and deepening risks for overdose and long-term health damage.
Pennsylvania now reports 90% of samples contain medetomidine, while counterfeit benzodiazepines (especially bromazolam) have replaced traditional prescriptions. In Oregon, coroners are finding carfentanil in fatal overdoses, and responders describe cases requiring four or more doses of naloxone to achieve reversal. Everywhere, polysubstance exposure is the norm, not the exception.
The Kratom Question: A Hidden Risk in Policy Shifts
Amid this chaos, many people have turned to 7-OH-mitragynine, an active alkaloid in kratom, as an alternative—either to manage withdrawal, self-treat chronic pain, or avoid returning to prescription opioids (or even to fentanyl). But if federal or state bans cut off legal access, thousands who depend on kratom to stay away from opioids will face a devastating choice: endure unmanaged withdrawal or return to a street supply now saturated with fentanyl, xylazine, benzodiazepines, and other adulterants.
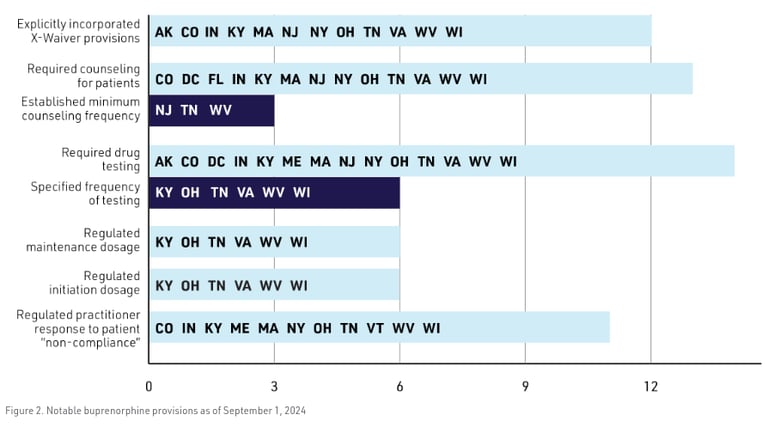
Ordinarily, this would be the moment to transition people to buprenorphine (Suboxone), one of the most effective tools for opioid use disorder. Despite the removal of the federal “X-waiver,” substantial barriers to buprenorphine access remain. Current federal policy still requires patients who have been receiving telehealth prescriptions for six months to complete an in-person visit, a requirement that disproportionately impacts individuals with limited transportation, financial instability, or difficulty locating a provider who is both available and willing to assist. In many states, additional regulatory restrictions exceed federal requirements, further narrowing treatment pathways. At the pharmacy level, large retail chains frequently decline to fill buprenorphine prescriptions originating from telehealth visits, even when such prescriptions comply with federal and state law. The irony is striking: the same corporate entities that once allowed widespread dispensing of OxyContin and other opioids now restrict access to one of the most evidence-based treatments for opioid use disorder. Compounding this are persistent challenges at the provider level, where stigma, liability concerns, and insufficient training contribute to ongoing reluctance to prescribe. As a result, federal reforms designed to expand access have not achieved their intended impact in practice. For individuals who might otherwise transition from kratom to buprenorphine safely, these systemic barriers increase the likelihood of returning to an illicit supply that is increasingly volatile and dangerous.
For someone trying to stabilize after kratom withdrawal, these roadblocks can be insurmountable. Instead of being welcomed into treatment, people find themselves locked out—and funneled back toward the most dangerous drug supply in American history.
The Irony of Restricted Access
There is a deep irony in this situation regarding how pharmacies are responding as I mentioned earlier. The very lawsuits that targeted chain pharmacies for over-dispensing OxyContin and fueling the opioid crisis have pushed those same companies into policies that now make lifesaving medications like buprenorphine harder to obtain. In correcting one wrong, we have created another: a system that withholds treatment from those most at risk while offering little alternative but relapse into a fentanyl-saturated market.
What This Means for People Who Use
For people actively using—or those dependent on kratom to avoid opioids—the reality is stark:
Kratom bans will push some back into the illicit supply.
And today’s supply is not heroin or diverted pills—it is fentanyl plus xylazine, medetomidine, or benzodiazepines.
Tolerance mismatches are deadly.
Shifting from kratom or managed Suboxone to fentanyl, even briefly, radically increases overdose risk.
Systemic barriers create relapse pathways.
Policy restrictions on buprenorphine make transitions into evidence-based treatment unnecessarily difficult.
What This Means for Providers
Clinicians and harm reduction workers now face overlapping crises:
1.) Managing overdoses where naloxone may be insufficient because of xylazine or medetomidine.
2.) Treating complex wounds from xylazine exposure.
3.) Supporting patients who want Suboxone but cannot access it due to state law, pharmacy policy, or provider hesitation.
The Bottom Line
The drug supply is no longer what it was—even five years ago. The shift is not just toward fentanyl, but toward fentanyl plus something else: xylazine, medetomidine, benzodiazepines, stimulants, and cutting agents of all kinds. For people who use drugs, this makes every dose a gamble. For those who have managed their use with kratom, looming bans may push them directly back into this high-risk supply.
At the same time, barriers to buprenorphine access show the tragic irony of our policy landscape: in trying to atone for the overprescribing that helped spark the opioid epidemic, we have made it harder to deliver the very medication that can save lives in the era of fentanyl.
Adding to the danger, the current data does not fully capture the emerging threat of nitazenes, a class of ultra-potent synthetic opioids. Testing for nitazenes is not yet routine, meaning their presence is likely under-counted. Early evidence suggests they are far more potent than fentanyl, highly reinforcing, and less responsive to naloxone, making overdoses more difficult—or even impossible—to reverse in some cases. If nitazenes continue to infiltrate the street supply alongside fentanyl, xylazine, and other adulterants, we could be facing a whole new wave of opioid-related harm.
The combination of kratom bans, restricted Suboxone access, and the rising presence of nitazenes creates a perfect storm: people seeking to avoid overdose may be funneled into a supply where every dose carries unprecedented risk. Unless we respond with urgency, compassion, and evidence-based strategies—including expanded access to treatment, harm reduction, and comprehensive drug checking—the drug supply will continue to outpace our interventions, leaving devastation in its wake.